The Merit-based Incentive Payment System (MIPS) impacts how medical providers get paid through Medicare. When asked what is MIPS in healthcare, it’s a program that rewards quality care while controlling costs. If you run a clinic or practice, understanding this system is crucial for your bottom line. MIPS evaluates clinicians in four key areas and determines whether you get a bonus or penalty on future Medicare payments. Let’s dive into what this means for your practice.
Understanding What Is MIPS In Healthcare: A Complete Overview
Many providers wonder what is MIPS in healthcare and how it affects them. MIPS replaces older programs like Meaningful Use and the Physician Quality Reporting System. It’s part of the shift away from fee-for-service toward value-based care in the medical field. The system measures your performance against peers and adjusts Medicare payments accordingly.
Think of it as a report card for your practice. CMS collects data on how well you’re serving patients, managing resources, and using technology. Your performance determines whether you receive a payment boost or reduction down the road. For many practices, this can mean thousands of dollars of difference in revenue.

The Four MIPS Performance Categories Explained
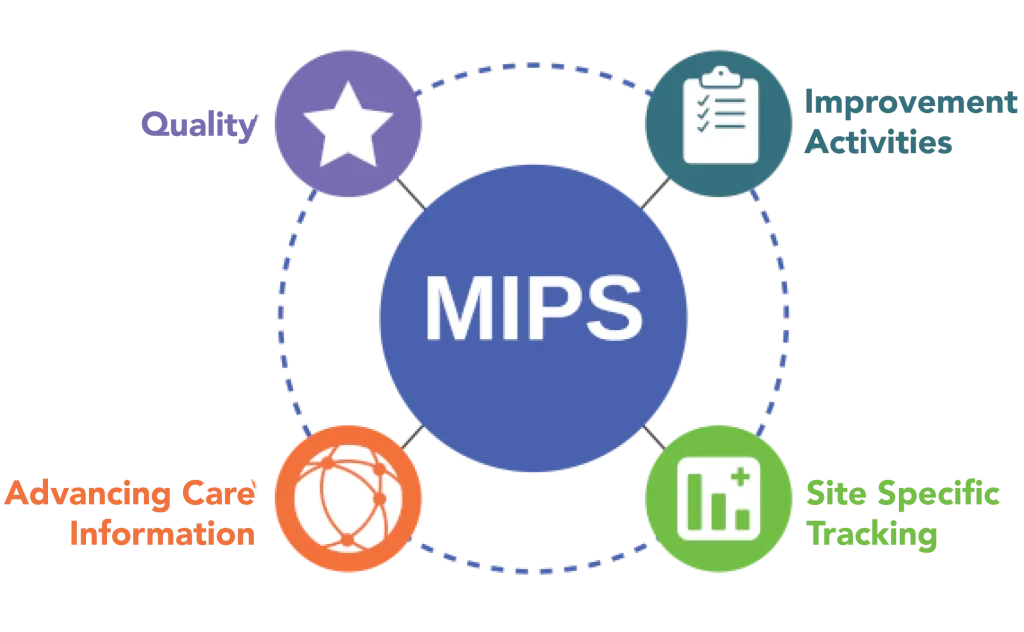
To fully understand what is MIPS in healthcare, you need to know its four main components. Each category examines a different aspect of your practice. They aren’t weighted equally, so some areas impact your score more than others.
Quality makes up 30% of your score and looks at the clinical care you provide. This includes things like preventive measures and patient outcomes. Cost also accounts for 30% and evaluates your resource use compared to similar providers. The system’s digital component, Promoting Interoperability, represents 25% and measures how effectively you use electronic records. Finally, Improvement Activities (15%) rewards efforts to enhance clinical practice.
- Reporting on at least six quality measures
- Having your cost efficiency evaluated through claims data
- Demonstrating meaningful use of certified electronic health record technology
- Implementing improvements in care coordination and patient engagement
How to Successfully Participate in MIPS Reporting
Getting started with reporting might seem overwhelming, but breaking it down makes it manageable. First, determine if you’re required to participate. Generally, if you bill Medicare more than $90,000 annually and see over 200 patients, you’re probably included.
When learning what is MIPS in healthcare, understanding reporting methods is key. You can report as an individual, a group, or through a special pathway called MVP (MIPS Value Pathway). Most clinicians use electronic health records or qualified registries to submit their data. Remember that for 2025, you need to report on at least 75% of eligible cases for quality measures – up from previous requirements.
MIPS Payment Adjustments and Their Impact on Your Clinic
Your performance directly affects your wallet. Scoring below the minimum threshold (currently 75 points) results in a penalty that could reach 9% of your Medicare payments. That’s significant money leaving your practice!
Exploring what is MIPS in healthcare reveals its financial implications. High performers receive positive adjustments. These aren’t just small bonuses – they can substantially boost your revenue, especially if you see many Medicare patients. Think about it: a practice with $500,000 in annual Medicare payments could gain or lose up to $45,000 based on their score. This system creates powerful financial incentives to focus on quality improvement.
Important Changes to MIPS in 2025 for Healthcare Providers
Several updates are coming for the 2025 performance year. The category weights remain stable (Quality 30%, Cost 30%, Promoting Interoperability 25%, and Improvement Activities 15%), providing some consistency in planning.
CMS has introduced seven new quality measures focused on diagnostics and public health priorities while removing ten outdated ones. If you run a small practice, you’ll benefit from simplified requirements – now needing just one improvement activity to earn maximum points in that category.
Cost scoring has been recalibrated against median thresholds, which might help boost scores for many participants. However, the stakes remain high with potential penalties affecting nearly 46% of solo practitioners and 21% of small practices.
Maximizing Your MIPS Score: Next Steps for Your Practice
Success in this system requires strategic planning. Start by reviewing your current performance data to identify weak spots. If quality scores are lagging, focus on implementing standardized protocols to improve consistency.
The final piece of what is MIPS in healthcare involves maximizing your score. Consider exploring the MIPS Value Pathway (MVP) option, which streamlines reporting for specialty-specific measures. This can reduce administrative burden while maintaining compliance.
Don’t go it alone – partner with experts who understand the complexities of the program. Whether through your EHR vendor or a specialized consultant, getting professional guidance can make a significant difference in your score and subsequent reimbursement.
FAQs
What are the benefits of MIPS programs?
MIPS programs boost revenue potential under the quality payment program while rewarding providers who deliver exceptional care. Eligible clinicians receive positive Medicare Part B payment adjustments based on performance, reduced reporting burdens compared to legacy programs, and data insights that improve patient outcomes and operational efficiency.
How do I find a quality reporting option for my MIPS final score?
Explore the QPP website for reporting options that fit your practice. Traditional MIPS offers flexibility for eligible clinicians to select quality measures and improvement activities. Consider your practice size, specialty, and reporting capabilities when choosing between individual, group, or MIPS APM reporting requirements.
What is a merit-based incentive payment system?
The merit-based incentive payment system, established through the Medicare Access and Chip Reauthorization Act, evaluates MIPS eligible clinicians across four performance categories.


